Mar 31, 2022
Researchers Identify New Targets for Immunotherapy in Colon Cancer
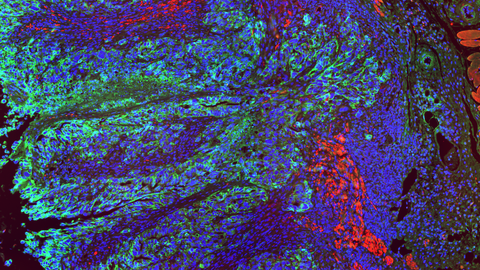
A multi-color image of colon tissue. Single cell nuclei are visible in blue. Colon cancer cells are highlighted in green. The cells infiltrate the organ lining and the muscle layers (red), ultimately leading to cancer cell migration into other organs.
Colon cancer is one of the most common types of cancer. Particularly in advanced stages of disease, the treatment still largely relies on traditional chemotherapy. The new generation of cancer treatments, so-called immunotherapies, has only been effective in a small subgroup of colon cancers. TU Dresden scientists led by Prof. Sebastian Zeissig have now identified proteins that are promising targets for new immunotherapies against colon cancer. Their results also underline the central role of intestinal bacteria in the development of colon cancer. The study was published in the journal Immunity on March 31, 2022.
Our bodies can naturally clear cancerous cells. Every day our immune system may detect mutated cells in our bodies and destroy them. Once in a while though, cancerous cells can find a way to hide from the immune system. The cells develop molecular signals that block immune cells from recognizing them as a threat. This, among other strategies, allows cancer cells to multiply and grow into tumors. Understanding the molecular mechanism of this process allowed for the development of new cancer treatments, the so-called immunotherapies. These treatments can unleash the patient’s immune system to target the tumor and limit its growth.
Unfortunately, current immunotherapies are not effective for all types of cancers. Most cases of colon cancer, one of the most commonly diagnosed type of cancer, do not respond to these treatments. Now, a team of researchers from TU Dresden described a new pathway that lets colon cancer hide from the immune system. Their results provide a potential first step towards the development of a new generation of immunotherapies.
How Colon Cancer Hides from the Immune System
Inhibition of immune cells is carried out by special signals present on the surface of cancer cells. “These signals are known as checkpoint proteins,” says Prof. Sebastian Zeissig from the University Hospital Dresden and the Center for Regenerative Therapies Dresden (CRTD) at TU Dresden who led the research team. Current immunotherapies use drugs called checkpoint inhibitors to target a small set of known checkpoint proteins. Unfortunately, this approach had only a very limited impact on colon cancer growth. “This raised the question of whether there are other checkpoint proteins that may represent more promising targets for immunotherapy in colon cancer,” says Dr. Kenneth Peuker, author of the study.
Researchers analyzed colon cancer samples and looked for signal proteins present in tumor cells but not in the healthy tissue. Two proteins caught their attention. CB7H3 and B7H4 were present in large number in colon cancer cells while almost undetectable in the healthy tissue.
“We decided to block B7H3 and B7H4 in colon cancer cells,” says Dr. Peuker. “The result was startling. Tumor tissue in which these signals were disabled showed significantly slowed growth or even shrinking. We have observed that now the immune cells could invade the cancer tissue and started to control tumor cells.” Additional tests confirmed that the B7H3 and B7H4 proteins are indeed working as checkpoint proteins. “Blocking these signals suddenly allowed immune system to attack tumor cells,” adds Prof. Zeissig.
Scientists found B7H3 and B7H4 to be present not only in the primary colon cancer tumors but also in their metastases in the liver. Turning these proteins off slowed the growth of the primary tumors but also their liver metastases. The team observed that some of the treated mice survived long-term despite having metastatic tumors.
Runaway Bacteria Block Immune Responses
The team characterized a broad cascade of events that allows colon cancer to develop its ability to block immune cells. They were able to show that breaking the intestinal barrier is a crucial step in the process. When the intestinal barrier breaks at sites of tumor development, bacteria that are normally present in the intestine can suddenly enter the surrounding tissue. This is considered an important early event in the development of colon cancer. Now, Prof. Zeissig’s team could show that these bacterial runaways serve as an initial trigger for the colon cancer cells to hide from the immune system.
“We found that cells present in the tissue can detect the invading bacteria. This, in turn, activates a full cascade of steps. The resulting molecular communication between the cells eventually leads the cancer cells to project B7H3 and B7H4 on their surface and hide from the immune system,” says Dr. Peuker.
The team could show that using broad-spectrum antibiotics to destroy the invading intestinal bacteria also reduced the tumor size and decreased the extent of liver metastases. “Our results provide a new link between microbiota and tumor growth in colon cancer. We would like to focus more on this angle in the future,” says Prof. Zeissig.
An artistic interpretation of the study results.
A Step Closer to New Colon Cancer Immunotherapies
The results of the new study come predominantly from research in mice but offer a promising outlook for future cancer therapies for humans. “Our analyses of human samples showed that B7H3 and B7H4 are also present in human colon cancer cells and that their presence correlates with poorer outcomes of colon cancer patients. These proteins are also barely detectable in healthy tissues in humans which suggests that their targeting may be safe,“ says Prof. Zeissig.
„We hope that our work will serve as a foundation for new studies that address the efficacy of targeting of B7H3 and B7H4 in human colon cancer in the future,“ adds Prof. Zeissig.
Original Publication
Kenneth Peuker, Anne Strigli, Daniele V. F. Tauriello, Alexander Hendricks, Witigo von Schönfels, Greta Burmeister, Mario Brosch, Alexander Herrmann, Sandra Krüger, Jessica Nitsche, Lea Južnić, Marc Marius Geissler, Andreas Hiergeist, André Gessner, Jakob Wirbel, Ruby Priyadarshini Ponnudurai, Antje Tunger, Rebekka Wehner, Daniel E. Stange, Jürgen Weitz, Daniela E. Aust, Gustavo B. Baretton, Marc Schmitz, Christoph Röcken, Jochen Hampe, Sebastian Hinz, Georg Zeller, Triantafyllos Chavakis, Clemens Schafmayer, Eduard Batlle, Sebastian Zeissig: Microbiota-dependent activation of the myeloid calcineurin-NFAT pathway inhibits B7H3- and B7H4-dependent anti-tumor immunity in colorectal cancer. Immunity (March 2022)
Link: https://doi.org/10.1016/j.immuni.2022.03.008
About the Center for Regenerative Therapies Dresden (CRTD)
The Center for Regenerative Therapies Dresden (CRTD) of TU Dresden is an academic home for scientists from more than 30 nations. Their mission is to discover the principles of cell and tissue regeneration and leverage this for the recognition, treatment, and reversal of diseases. The CRTD links the bench to the clinic, scientists to clinicians to pool expertise in stem cells, developmental biology, gene-editing, and regeneration towards innovative therapies for neurodegenerative diseases such as Alzheimer's and Parkinson's disease, hematological diseases such as leukemia, metabolic diseases such as diabetes, retina and bone diseases.
The CRTD was founded in 2006 as a research center of the German Research Foundation (DFG) and funded until 2018 as a DFG Research Center, as well as a Cluster of Excellence. Since 2019, the CRTD is funded by the TU Dresden and the Free State of Saxony.
The CRTD is one of three institutes of the central scientific facility Center for Molecular and Cellular Bioengineering (CMCB) of the TU Dresden.
Web: www.tu-dresden.de/cmcb/crtd
Web: http://www.tu-dresden.de/cmcb
Resources:
Website of Prof. Dr. med. Sebastian Zeissig’s group: https://tud.link/4sdb
Full resolution pictures: https://tud.link/uus6
Scientific contact:
Prof. Dr. med. Sebastian Zeissig
Medizinische Klinik I - Universitätsklinikum Dresden
Center for Regenerative Therapies Dresden (CRTD)
Technische Universität Dresden
Fetscherstr. 105, 01307 Dresden
Tel: +49 351 458-19171
Email:
