inCare - The Intelligent Case Record
Digital patient pathways as an element of the intelligent electronic health record – Technology development and testing using telemedical applications in geriatric care
Background
Complex geriatric symptoms are now regarded as one of the major challenges associated with the ageing of the population. Shortage of time, incorrect and poorly documented admission assessments as well as insufficient information about previous treatment steps are examples of the many immediate problems faced by service providers in geriatric care. To alleviate some of these problems, systematic patient training and education are needed. As a result of these and other causes, an increased risk of patients falling down and injuring themselves can currently be observed. This is associated with an increased risk of hospital stays and the need for long-term care. Clinical documentation systems are not designed to support coordination in integrated care settings. Instead, inter-organizational and inter-sectoral care is not centrally managed and informational patient participation is not sufficiently provided for. Thus, the following core problems can be identified:
1. Low regional coordination within defined care complexes, such as geriatric care for patients who have a high risk of falling down and injuring themselves.
2. Low information integration and evaluation of integrated care models.
3. Lack of established and monitored process standards in terms of treatment pathways.
4. Inadequate provision of digital information for the patient beyond the legal minimum requirements (i.e. in addition to hard copies of doctor's letters or the expected requirements of the German Digital Healthcare Act).
Objectives
The focus of the inCare project is the digital implementation of an integrated, geriatric stroke patient pathway. This will be used for prevention, identification and needs-based, cross-sectoral, coordinated care of geriatric patients who have a high risk of falling down. For this purpose, a model solution is to be created for the identification of the complex symptoms of such geriatric patiens. This will improve adherence to therapy and guideline compatibility, as well as the realization of needs-based information transfer. In addition to service providers, this technological basis should enable patients to be involved in the patient pathway and thus also create a value-added application for the future telematics infrastructure. For the service providers involved (general practitioners, nursing, specialists), an informational foundation will also be created, which will enable improved coordination and, in particular, better evaluation of care. In this context, existing documentation systems will be integrated into the entire patient pathway. An integrated pathway evaluation system will be implemented as part of an "intelligent" electronic health record, and the evaluation will be processed. In addition to structured and semantically defined progress documentations, this electronic health record will also provide comparative information that can be obtained on the basis of the evaluation of similar or identical care processes using Big Data approaches. Thus, the aim is to extend the documentation, which is in any case necessary, and evaluate and process cross-treatment primary and secondary data for patients and service providers using artificial intelligence technology.
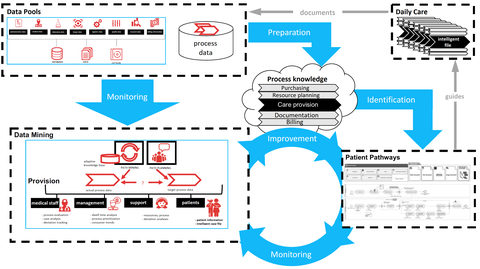
Figure 1: Interdependencies of integrated patient pathways and data mining of an intelligent electronic health record
These measures provide for the identification, consolidation and path-based evaluation of existing and pre-existing process knowledge of daily care practice within the documentation data that is generated. Up until now, this essential information (in particular the implicit process knowledge about the total amount of care data) is rarely fully known or available to the participants involved. For this purpose, as illustrated in Figure 1, various documented activities from a wide variety of data pools and systems must be collected and analysed. In order to control the quantity and heterogeneity of the partly structured and partly unstructured information, data mining methods and systematics from the field of artificial intelligence are used. In addition, the care data must be prepared for specific target groups and treated with integrity in terms of data protection. Therefore, the preparation and provision of clinical case documentation for the patient or his relatives is an essential focus of the measure (monitoring via patient portal/patient app). Conversely, the resulting system and database also provides important information to the service provider for the active control of risk factors along the patient pathway and thus, also contributes as a component of integrated quality management. This potential benefit is expressed both at the case level of individual care services (monitoring) and at the meta-level of integrated care of geriatric patients who have a high risk of falling down through a continuous evaluation of the patient pathways (improvement).
Sponsored by:
 © Carl Gustav Carus
© Carl Gustav Carus
 © Symate
© Symate
Contact: Dr. Martin Burwitz