Sep 11, 2024
Development of novel hPS reporter cell lines for the improvement of diabetes stem cell therapies
Human pluripotent stem (hPS) cells can differentiate into any cell type in the human body, including pancreatic islet cells. The current methods used to differentiate hPS cells into mature, insulin-producing beta cells are not efficient or consistent enough to be used for diabetes cell therapies. In this new study, published in Scientific Reports, researchers from the Paul Langerhans Institute Dresden (PLID) of the German Center for Diabetes Research, have developed hPS cell fluorescent reporter lines that can be used to monitor the progress and efficiency of the differentiation into functional pancreatic islet cells.
Pancreatic beta cells produce insulin, the hormone that regulates the uptake of glucose from the blood into the cells of the body. The loss or impaired function of these cells leads to diabetes, a disease in which the body cannot produce sufficient amounts of insulin. Current treatments, particularly for type 1 diabetes, include insulin injections or pancreas transplants, but these therapies have their limitations. Another possible future diabetes therapy would be the use of pancreatic islet cells, including insulin-producing beta cells derived from hPS cells. The use of hPS cells for diabetes cell therapies would be able to overcome the limitations of current treatments. However, the process of differentiation of hPS cells into beta cells is currently not well enough understood. Furthermore, it will be necessary to improve the current differentiation methods for the production of mature, insulin-producing cells.
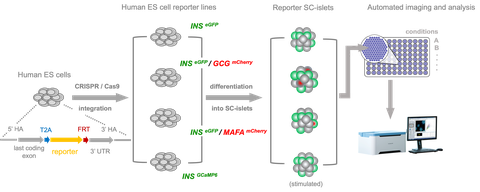
To follow the differentiation process, the researchers in this study used CRISPR-Cas9 gene editing. “We created hPS cell reporter lines in which fluorescent proteins reflect the expression of key islet-specific proteins such as the hormones insulin (INS) and glucagon (GCG) and the transcription factor MAFA,” explains Prof. Anthony Gavalas, lead author of the study. “Visualizing these proteins allowed us to follow the development and maturation of different islet cell types in real time, giving us a detailed insight into the differentiation process.” The researchers used these lines and created an automated high-throughput imaging pipeline that helped to identify a new additive called N21, which is able to increase the number of insulin-producing cells.
The ability to reliably produce functional beta cells from hPS could reduce reliance on insulin injections or pancreas transplants, providing a more sustainable and effective treatment option for people with type 1 diabetes. “The hPS cell reporter lines and the high-content live imaging approach described in this study allow efficient assessment of the various conditions for optimal islet cell differentiation and maturation, including functional beta cells,” concludes Prof. Gavalas. The use of advanced genetic engineering techniques and real-time imaging thus paves a new path for future innovations in the treatment of diabetes and related diseases.
Original publication:
Elisa Zanfrini, Manuj Bandral, Luka Jarc, Maria Alejandra Ramirez-Torres, DanielaPezzolla, Vida Kufrin, Eva Rodriguez-Aznar, Ana Karen Mojica Avila, Christian Cohrs, Stephan Speier, Katrin Neumann, Anthony Gavalas (2024). Generation and application of novel hES cell reporter lines for the differentiation and maturation of hPS cell-derived islet-like clusters. Sci Rep 14, 19863 (2024). https://doi.org/10.1038/s41598-024-69645-4