Research Focus
Islet of Langerhans physiology in the pathogenesis and therapy of diabetes
Background
Diabetes is a growing epidemic with major impact on life style, health and life expectancy of the affected patients. Diabetes develops when systemic insulin concentrations are insufficient to control blood glucose homeostasis. This shortage in insulin is either caused by a functional deterioration of insulin secreting pancreatic beta cells or by a loss of their mass (reduced cell number). Recent research by our and other groups has shown that in different phases of type 1 and type 2 diabetes pathogenesis the contribution of changes in beta cell mass and/or function varies (Figure 1).
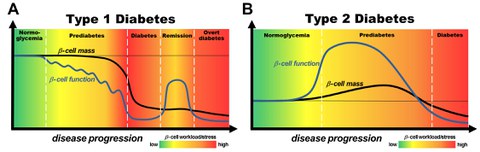
Figure 1. Models of the contribution of beta cell mass and function to pathogenesis of type 1 diabetes (A) and type 2 diabetes (B). Black line: beta cell mass; Blue line: beta cell function. The color-coded background indicates the intensity of beta cell workload and stress caused by insulin resistance, metabolic demand, hyperglycemia and additional cytotoxic factors. From: Chen, C., Cohrs, C.M., Stertmann, J., Bozsak, R., and Speier, S. (2017). Human beta cell mass and function in diabetes: Recent advances in knowledge and technologies to understand disease pathogenesis. Mol Metab 6, 943-957.
Based on these findings we believe that successful treatment of diabetes depends on targeting beta cell dysfunction and mass loss in specific phases of pathogenesis. Thus, our group investigates the role of beta cell mass and function at distinct stages of diabetes pathogenesis and aims to discover novel therapeutic targets for beta cell protection and recovery in type 1 and type 2 diabetes. A central aspect of our research is the translation of our findings into the human setting by utilizing novel platforms to study human pancreatic tissue and islets. In addition, we utilize our unique platforms to optimize alternative cell sources for the successful generation of cell replacement therapies for diabetes.
Approach
The unique approach of our lab is the study of islet cell physiology within an intact tissue environment or the systemic setting. For that purpose we have established novel in situ and in vivo techniques to complement standard methods of islet research. Thereby, we aim to account for the numerous local and systemic signals which affect the physiology and pathogenesis of islets within the organ tissue and inside the living organism.
For example, the pancreas tissue slice platform allows us to study the human pancreas from organ and tissue donors to assess for the first time human islet cell pathophysiology within an intact organ tissue environment.
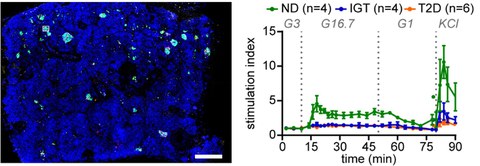
Figure 2. Left: Maximum intensity projection of a human pancreas tissue slice stained with antibodies against insulin (green), glucagon (magenta), and somatostatin (grey) counterstained with DAPI (blue). Scale bar, 500 mm. Right: Insulin secretory pattern of pancreas tissue slices from non-diabetic (ND) (green), impaired glucose tolerant (IGT) (blue), and type 2 diabetic (T2D) (orange) donors during perifusion. From: Cohrs, C.M., Panzer, J.K., Drotar, D.M., Enos, S.J., Kipke, N., Chen, C., Bozsak, R., Schoniger, E., Ehehalt, F., Distler, M., Brennand, A., Bornstein, S.R., Weitz, J., Solimena, M., and Speier, S. (2020). Dysfunction of Persisting beta Cells Is a Key Feature of Early Type 2 Diabetes Pathogenesis. Cell Rep 31, 107469.
In addition, our in vivo imaging platform facilitates the noninvasive longitudinal observation of islet physiology in a systemic setting for prolonged time periods. This unique setup enables for the first time to study islet cells during changing metabolic conditions and disease pathogenesis.
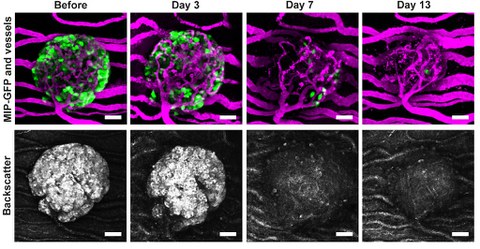
Figure 3. Longitudinal in vivo observation of islet destruction during type 1 diabetes progression. Green: beta cells; Magenta: blood vessels; Grey: cell lightscatter. From Chmelova, H., Cohrs, C.M., Chouinard, J.A., Petzold, C., Kuhn, M., Chen, C., Roeder, I., Kretschmer, K., and Speier, S. (2015). Distinct roles of beta-cell mass and function during type 1 diabetes onset and remission. Diabetes 64, 2148-2160.
Current Projects (examples)
- Mechanisms of islet cell dysfunction in type 2 diabetes pathogenesis
- Optimization of stem cell based and xenogeneic alternative cell sources for transplantation therapy
- Endocrine-immune cell interactions in type 1 diabetes
