Research Focus
Hypertension-related organ damage - pathophysiology, treatment, and gender differences
Chronically elevated blood pressure (hypertension) is the leading cause of morbidity and mortality worldwide. Currently, more than one billion people worldwide have hypertension. Hypertension ultimately causes damage to target organs such as the heart, blood vessels, kidneys and brain, increasing the risk of stroke, heart attack, chronic kidney disease and dementia. Current treatment focuses mainly on lowering arterial blood pressure, which does not correspond to causal therapy.
Our research involves three main aspects:
Metabolic changes in endothelial cells and adipocytes and their contribution to organ damage in hypertension
Dysfunction of various cells contributes to organ damage in hypertension, which promotes further progression of hypertension. Pathological changes in homeostatic functions of cells and their dysfunction are inconceivable without metabolic changes in these cells. Here, we are interested in the metabolic remodeling of endothelial and perivascular adipocytes in hypertension. In particular, we are studying the mechanisms that contribute to these metabolic changes and investigating their relevance to cellular dysfunction and organ damage in hypertension.
Experimental anti-inflammatory strategies to search for new targets to treat organ damage
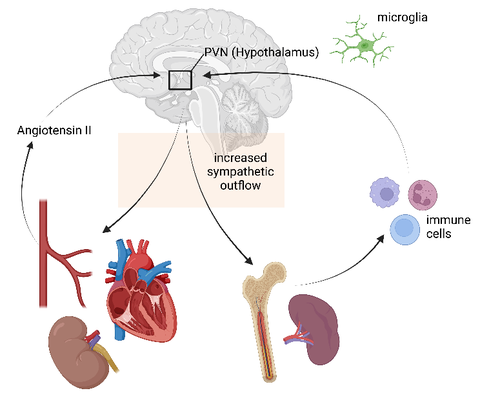
Fig. 1: Neuro-immune crosstalk and its contribution to hypertensive organ damage. (biorender.com)
There is strong evidence that the immune system plays a causative role in the development of hypertension and associated target organ damage. A complex neuro-immune crosstalk between the CNS and peripheral organs such as the spleen and bone marrow has been implicated in hypertension. For example, increased sympathetic tone activates peripheral immune cells that, together with hypertensive stimuli such as angiotensin II (ANGII), can trigger microglial activation and neuroinflammation in the brain. Activated microglia can then further increase sympathetic activity, directly influencing hypertension and organ damage.
Therefore, we are exploring mechanisms of immunomodulation to find new targets for hypertension therapy
Mechanisms of gender differences in hypertension and the cardiovascular system
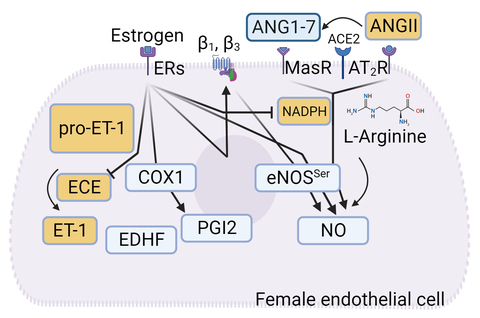
Fig. 2: Estrogen-dependent regulation of β-adrenoceptor expression and endothelial function.
There are sex differences in the development of hypertension and associated organ damage. While women develop hypertension later in life compared with men of the same age, the consequences of cardiovascular complications may be worse in women. These differences are largely attributed to sex hormones. We are investigating the sex-dependent expression of endothelial β1- and β3-adrenoceptors and their role in the development of hypertension and organ damage. We have shown that estrogen, but not other sex hormones, regulates the expression of these adrenoceptors. Therefore, we are investigating estrogen receptors and the downstream signaling cascade in the regulation of endothelial β1- and β3-adrenoceptors.
In addition to hypertensive cardiac hypertrophy, we are also investigating the mechanisms regulating cardiac contractility. Here, we use a mouse model in which systolic dysfunction develops shortly after induction of a gene knockout. These models of cardiac dysfunction require extensive in vivo studies of cardiac function. Using the Vevo3100 imaging system from FUJIFILM VisualSonics, we are able to assess dimensions of cardiac structures in different cross-sectional images, as well as determine systolic and diastolic functional parameters.
Fig. 3: Echocardiography of mouse heart
Methods:
- Implantation of osmotic minipumps (e.g., for continuous angiotensin II infusion)
- Non-invasive blood pressure measurement
- Histology
- Immunofluorescence
- Mulvany myography
- RT-qPCR, Western blot
- Echocardiography
- Flow cytometry
- Metabolomics
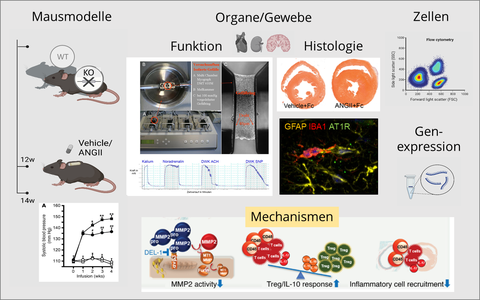
Fig. 4: overview of workflow and methods. DEL-1 mechanism see Failer T & Amponsah-Offeh, M et al. J Clin Invest. 2022;132(6):e126155 https://doi.org/10.1172/JCI126155 (biorender.com)
