Jul 28, 2023
The bidirectional relationship of viral infections and metabolic diseases
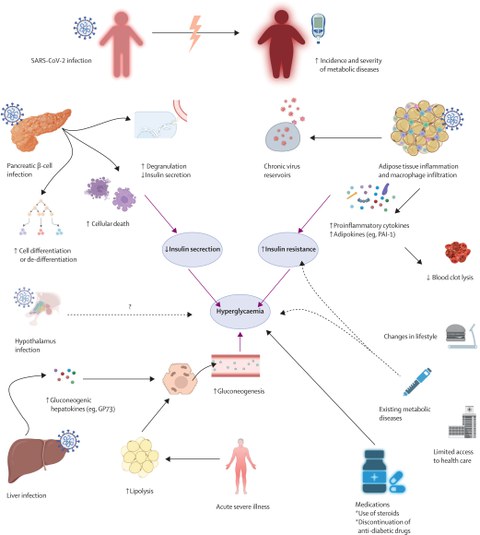
Factors contributing to the development or aggravation of diabetes in patients with SARS-CoV-2 infection
Viruses have been present during all evolutionary steps on earth and have had a major effect on human history. Today, a public health concern is the increase of non-communicable metabolic diseases in the last four decades. A group of scientists from the Paul Langerhans Institute Dresden (PLID) teamed up with international experts in the field to revisit the scientific evidence supporting the presence of a strong bidirectional feedback loop between several viral infections and metabolic diseases. The review is published in the renowned journal Lancet Diabetes Endocrinology, and discusses how viruses might lead to the development or progression of metabolic diseases and conversely, how metabolic diseases might increase the severity of a viral infection.
Viruses are infectious, non-autonomously replicating biological agents that exist in many varieties and have been present in all evolutionary steps of life on earth. Not only the SARS-CoV-2 pandemic, but also Spanish influenza or the HIV epidemic have had a major effect on societal development. The emergence and spread of old and new viral infections are associated with major transitions in the relationships of humans with the natural environment. Especially these days, mankind is experiencing a new transition period reflecting the effect of environmental, technological, demographical, and behavioral changes occurring in human societies spread.
Since decades scientists observe the development of non-communicable global epidemics of metabolic diseases, characterized by continuously increasing prevalence of obesity, type 2 diabetes (T2D) or non-alcoholic fatty liver disease. And already today, the consequences of non-communicable epidemics on affected societies are tremendous. For example, diabetes is the ninth leading cause of death and an important risk factor of four other top-ten leading causes of mortality (ischemic heart disease, stroke, chronic obstructive pulmonary disease, and kidney diseases).
“Within our new review, we revisit the scientific evidence supporting the presence of a bidirectional relationship between several viral infections and metabolic diseases. Our aim is not to provide a comprehensive list of all the available data, but to present the current knowledge about some principle mechanisms explaining this relationship and to discuss the most intriguing new concepts”, says Prof. Nikolaos Perakakis, PLID research group leader and corresponding first author of the article. “Regarding metabolic diseases, we focussed on diabetes, both type 1 and type 2 as well as fatty liver disease. We selected these metabolic diseases because of their high prevalence, their considerable health care burden, and the level of scientific data linking them with viral infections.”
Viruses promote metabolic diseases – or not?
It is known from several studies that viruses promote metabolic diseases by affecting important cell functions such as the regulation of cell survival and specific pathways pertinent to cell death, proliferation, or dedifferentiation in key endocrine and metabolic organs. Moreover, viruses are capable of controlling cell glucose metabolism by modulating glucose transporters altering glucose uptake, regulating signaling pathways involved in cellular energy sensing and stimulating glycolysis in infected cells.
Mostly enteroviruses, but also mumps, parainfluenza virus or human herpes virus 6 have been associated with the development of diabetes due to beta cell destruction. The timing of infection often precedes or coincides with the peaks in development of islet autoantibodies that occur at age 2 for insulin autoantibodies and between 3–5 years of age for glutamic acid decarboxylase autoantibodies. However, only a small proportion of the population will eventually develop type 1 diabetes, suggesting an important role for factors, such as genetic background or timing of infection.
Infection with hepatitis C virus (HCV) has been associated with an increased risk for the development of type 2 diabetes, and it is even higher in older people with a family history of diabetes. The detrimental effects of HCV on glucose homeostasis are primarily attributed to increased hepatic insulin resistance. HCV reduces hepatic glucose uptake by downregulating the expression of glucose transporter and additionally impairs insulin signaling by inhibiting the PI3K/Akt pathway.
Metabolic diseases affect severity of viral infections
People with obesity, insulin resistance, or diabetes display considerable alterations in both innate and adaptive immune system functions. Regarding the innate immune system, impaired chemotaxis, and phagocytosis of neutrophils have been observed in patients with type 2 diabetes. Regarding the adaptive immune system, in obesity, natural killer T cell numbers decrease in the adipose tissue, whereas B cells accumulate in adipose tissue and secrete more proinflammatory cytokines. Longitudinal multiomics analyses of diverse biospecimens from people with insulin resistance presented a delayed immune response following respiratory viral infections compared with people with normal insulin sensitivity. And also, hyperglycaemia appears to be an important mediator of diabetes-induced memory CD8 T-cell dysfunction in viral infections. All these alterations can contribute to a delayed and impaired immune response after infection that results in faster viral replication and longer viral shedding.
“It is obvious, that a considerable lack of information remains regarding the mechanisms governing the bidirectional relationship between metabolic diseases and viral infectious diseases”, concludes Perakakis. “Thus, it will be important to train a new generation of scientists, clinicians, and health-care personnel with a combined knowledge in both the fields of metabolic and infectious diseases to allow further understanding of the complex cross-specialty scientific questions in a timely manner. This will lead to more effective preventive and treatment strategies aiming to improve overall health, while simultaneously preparing us for future pandemics.”
Importantly, Dresden has a long-standing tradition in investigating the bidirectional relationship between metabolic diseases, inflammation and infections. This is reflected by studies of several research groups at PLID, for example the work of Prof. Stefan Bornstein's group on SARS-CoV2 infections, Prof. Michele Solimena's group on type 1 diabetes and coxsackievirus infections, or Prof. Triantafyllos Chavakis' group on trained immunity in metabolic diseases. Together with their colleagues in Zürich, who participated in this review, the Dresden scientists aim to further investigate different aspects of this bidirectional relationship in future studies. This will create a unique hub of combined expertise and excellence in this important research area.
Original publication:
Perakakis N, Harb H, Hale BG, Varga Z, Steenblock C, Kanczkowski W, Alexaki VI, Ludwig B, Mirtschink P, Solimena M, Toepfner N, Zeissig S, Gado M, Abela IA, Beuschlein F, Spinas GA, Cavelti-Weder C, Gerber PA, Huber M, Trkola A, Puhan MA, Wong WW, Linkermann A, Mohan V, Lehnert H, Nawroth P, Chavakis T, Mingrone G, Wolfrum C, Zinkernagel AS, Bornstein SR. Mechanisms and clinical relevance of the bidirectional relationship of viral infections with metabolic diseases. Lancet Diabetes Endocrinol. 2023 Jul 28:S2213-8587(23)00154-7. doi: 10.1016/S2213-8587(23)00154-7.
