Jan 31, 2022
A single-cell atlas of beta-cell regeneration reveals a new population of cells that helps zebrafish to recover from diabetes
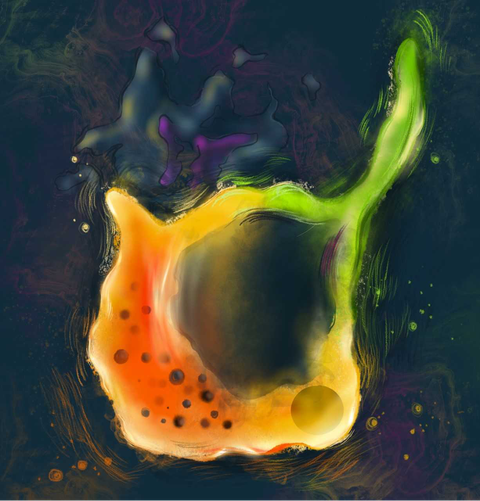
An artist’s representation of a hybrid cell, which is in part beta and in part delta cell.
Zebrafish can recover from diabetes by regenerating the insulin-secreting beta cells in the pancreas. However, the cellular dynamics underlying this capability remain unexplored. To overcome this knowledge gap, scientists from the Paul Langerhans Institute of the Helmholtz Zentrum München at the University Hospital Carl Gustav Carus and Faculty of Medicine of TU Dresden (PLID) teamed up with groups from ULB Bruxelles and MDC Berlin. The researchers used single-cell transcriptomics to map de novo beta cell regeneration during induction and recovery from diabetes in zebrafish. This recently published work in the renowned journal “Development” provides an atlas of beta cell regeneration, identifying a previously unknown population of glucose responsive hybrid cells, which plays an important role for the resolution of diabetes in zebrafish.
The pancreas is composed of two distinct parts, namely the exocrine and endocrine compartments. The exocrine part is involved in food digestion via the function of acinar and ductal cells. The endocrine compartment is instead responsible for maintenance of blood glucose homeostasis and is organized into the islets of Langerhans, which consist of three major cell types: alpha, beta and delta cells. To regulate this process, the three cell types produce and secrete specific hormones: alpha cells generate glucagon, beta cells generate insulin and delta cells generate somatostatin. Blood glucose homeostasis is achieved by regulated secretion of endocrine hormones in the blood stream; insulin activates glucose uptake in peripheral tissue, while glucagon opposes insulin action by stimulating the production of sugar in the liver. Somatostatin release has an inhibitory role for both insulin and glucagon secretion. As the selective autoimmune destruction of beta cells causes type-1 diabetes, enhancing the limited regenerative potential of the pancreas has become an important quest towards developing new regenerative therapies.
In this study, the team of Prof. Nikolay Ninov (PLID) applied a unique blend of in vivo imaging, single-cell genomics and genetics to study de novo beta cell regeneration in zebrafish. “Although regeneration is incomplete in mammals, zebrafish can naturally recover from extreme beta cell destruction and hyperglycemia, which make them an interesting and helpful model organism to uncover the principles of regeneration”, explains Prateek Chawla, PhD student in the International Research Training Group 2251 "Immunological and Cellular Strategies in Metabolic Disease" (ICSMD) of the Technical University of Dresden and King's College London and one of the first authors of the study. By categorizing the cells in the zebrafish pancreas, the team found that the zebrafish islet contains two discrete populations of delta cells. Moreover, the scientists found a subset of islet cells existing under a hybrid identity. They are sharing the hormones and fate determinants of both delta and beta cells. Interestingly, during ablation and subsequent regeneration, these hybrid cells form de novo, acquire glucose responsiveness and serve as a major source of insulin expression. “We therefore believe that the rapid formation of glucose-responsive hybrid cells can provide a shortcut to restoring glucose homeostasis and contributes to the ability of zebrafish to reverse the course of diabetes.” says Prof. Ninov.
In more detail, the group used single-cell sequencing to characterize cellular dynamics in a regeneration-competent zebrafish. Thereby, the gene expression of different pancreatic cells upon beta cell destruction was defined, which subsequently allowed the establishment of an “beta cell regeneration atlas”, spanning the period from beta cell destruction to emergence of new insulin-expressing cells. This atlas is now publically available, making it possible to examine the gene-expression of each cell type in a curated online database. Notably, the single-cell resolution of the analysis allowed the identification of the bi-hormonal cells with hybrid cell identities, which help the fish to restore normoglycemia even after near-complete beta cell ablation. In addition, this work discovered a specific protein that can promote the formation of such bi-hormonal cells when its expression levels are elevated genetically in zebrafish.
“One of the take-home messages of our study is that regenerating imperfect yet functional hybrid cells capable of insulin-production may offer the opportunity to elicit glucose control.” summarizes Ninov. “Perhaps, such surrogate cells would be stealthy in terms of escaping immune cell recognition and destruction in type-1 diabetes, as they exist under a hidden identity, resembling two different hormonal cell types at the same time.” The next step will be to find out if such cells exist and can be expanded in the human pancreas. The Ninov group will collaborate with the scientists from PLID who have established new systems to study human islets from donors. The ultimate goal is to apply the lessons learned from zebrafish in order to enhance the regeneration of human beta cells as a regenerative therapy for type-1 diabetes.
Original Publication:
Singh SP, Chawla P, Hnatiuk A, Kamel M, Silva LD, Spanjaard B, Eski SE, Janjuha S, Olivares-Chauvet P, Kayisoglu O, Rost F, Bläsche J, Kränkel A, Petzold A, Kurth T, Reinhardt S, Junker JP, Ninov N. A single-cell atlas of de novo β-cell regeneration reveals the contribution of hybrid β/δ-cells to diabetes recovery in zebrafish. Development. 2022 Jan 15;149(2):dev199853. doi: 10.1242/dev.199853. Epub 2022 Jan 28.
Contact:
Prof. Nikolay Ninov, PhD
Paul Langerhans Institut Dresden des Helmholtz Zentrums München am Universitätsklinikum und der Medizinischen Fakultät Carl Gustav Carus der TU Dresden
Fetscherstraße 74, 01307 Dresden
Email: nikolay.ninov@tu-dresden.de
