Oct 27, 2021
Post-COVID: Analysis of health insurance data shows possible long-term health implications of COVID-19, including in children and adolescents
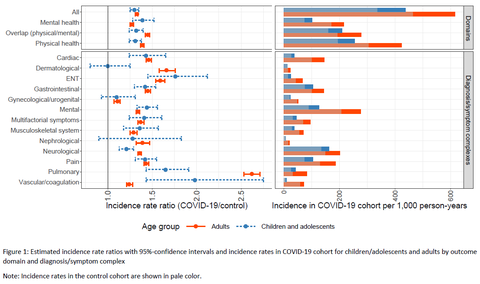
COVID-19 patients were more likely to receive a medical diagnosis of physical or psychological symptoms and illnesses more than three months after acute infection than those who were not diagnosed with COVID-19, according to an extensive study of health insurance data. In addition to adults, children and adolescents are also potentially affected by post-COVID: The most documented symptoms and illnesses related to COVID-19 among children and adolescents include feeling unwell, sudden fatigue, cough, sore throat and chest pain as well as anxiety and depression. Common medical diagnoses in adults included loss of taste, fever, cough and respiratory problems. Several German public health insurers participated in the study, which has been coordinated by the Center for Evidence-Based Healthcare (ZEGV) at Dresden University Hospital and the Robert Koch Institute. The findings have been published in a preprint (“Post-COVID in children, adolescents, and adults: results of a matched cohort study including more than 150,000 individuals with COVID-19” https://www.medrxiv.org/content/10.1101/2021.10.21.21265133v1).
“Internationally, this is one of the first and largest controlled cohort studies on post-COVID. Our partners’ extensive database and innovative methodical procedure have facilitated reliable conclusions about the long-term consequences of COVID-19 in children and adolescents for the first time,” said Prof. Dr. Jochen Schmitt of University Hospital Dresden. More research is needed to understand the links between COVID-19 and these illnesses. “Future analyses should focus on the persistence of possible health problems among the participants of the study. It is also crucial to investigate how applicable these results are to subsequent phases of the pandemic and associated changes in care conditions,” adds Dr. Martin Rößler from Dresden University Hospital.
Post-COVID comprises persistent or newly developed symptoms of illness and health problems in the long term (at least three months subsequent to infection with SARS-CoV-2). However, it remains unclear what exactly characterizes post-COVID and how many people are affected by it. Addressing this question relies on controlled studies which observe the current health of SARS-CoV-2 patients over a sufficiently long period, and compare their data with a well-defined control group. Previous international studies of this kind indicate an impact on adults’ health in the long term. This analysis by ZEGV, RKI and the health insurance providers has now provided new insights on post-COVID in younger age groups based on data from German health insurance providers. The data used for the study was the billing data from 2019 and 2020 of about 38 million public insurance holders from AOK Bayern, AOK PLUS Sachsen and Thüringen, BARMER, DAK-Gesundheit, Techniker Krankenkasse and the research database InGef, from which a significant portion of the data from company health insurance funds was extracted. The analysis included data from over 150,000 individuals who were diagnosed with COVID-19 by a medical laboratory in the first half of 2020, 12,000 of whom were children and adolescents. For each infected person, five non-infected insurance holders of comparable age and sex, and with comparable pre-existing medical conditions were included in the study for a similar follow-up period. Infected and non-infected individuals were collated with regard to 96 predefined symptoms and conditions, which were newly documented three months subsequent to the date of infection/inclusion in the study.
The analyses demonstrated that new symptoms and conditions were more commonly diagnosed in adults, children and adolescents more than three months after a positive COVID-19 diagnosis than in comparable persons belonging to the control group. The newly documented diagnoses concern both physical and mental illnesses as well as many different organ systems and symptom complexes. With regard to all of the symptoms and illnesses analyzed, the prevalence of newly documented illness was approximately 30% higher in children and adolescents who had previously been diagnosed COVID-19 as in those who had not been diagnosed with COVID-19. The study compared diagnosis rates based on 1,000 person-years, taking into consideration the different follow-up observation periods for the individuals included in the study. The rate of diagnosis in children with COVID-19 was about 437; for children not diagnosed with COVID-19, it was about 336. At around 616, the rate of diagnosis with other illnesses in adults previously diagnosed with COVID-19 was approx. 33% higher than that of the control group without COVID-19 at 464. Overall, children and adolescents were less frequently affected than adults.
The study is part of the “Post-COVID-19 Monitoring in Routine Health Insurance Data” (POINTED) project. Earlier analyses examined risk factors for severe cases of COVID-19 based on health insurance provider data (see the publication in EpidBull 19/2021 https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2021/19/Art_02.html).
Contact:
Center for Evidence-Based Healthcare, Carl Gustav Carus University Hospital and Medical Faculty of TU Dresden
Autors of the Analysis:
Dr. Martin Rößler/Prof. Jochen Schmitt
Email: (for establishing contact directly)
Tel.: +49 351 458-89211 (Secretary’s Office)
Press Office of the Carl Gustav Carus University Hospital:
Email:
Tel.: +49 351 458-4162