State of the art science
In type 1 and type 2 diabetes, destroyed or impaired beta cells cause an elevated blood sugar level. PLID scientists are working on deciphering the mechanisms that lead to the destruction and/or functional impairment of beta cells and are also trying to develop new approaches to replace damaged or destroyed beta cells.
 © Andreas Müller
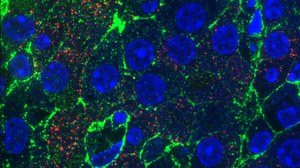
© Andreas Müller
Research at the Paul Langerhans Institute Dresden
For this purpose, we use innovative research approaches and state-of-the-art methods to investigate the different aspects of the disease.
For instance, scientists investigate the molecular basis of the formation, storage and secretion of the insulin granules in which the beta cells store the insulin. At the same time, we are investigating the lipid composition of the beta cell plasma membrane in order to understand how modifications in its composition, e. g. after the exocytosis of insulin granules, influence the signalling properties of membrane receptors. Through close cooperation with the clinic for visceral, thoracic and vascular surgery (VTG) we are able to identify the genetic, epigenetic and physiological characteristics of human pancreatic islets, i.a. of metabolically phenotyped non-diabetic, prediabetic and diabetic subjects with the aim to understand the molecular changes associated with beta and alpha cell dysfunction along the natural history of type 2 diabetes. The integration of these data with medical records and clinical-chemical laboratory data should subsequently enable the identification of reliable biochemical biomarkers for the progression of type 2 diabetes.
Within highly translational research approaches, PLID scientists and physicians are working on therapies to replace or regenerate damaged and already destroyed beta cells. They are using regeneration models in mice and zebrafish and are working on the auto- and allogeneic transplantation of insulin-producing islet cells from human donors. In the future, animal tissues (Xenotransplantation) or inducible pluripotent stem cells will also serve as a source for the transplants.
The clinically active research groups of the PLID are amongst others involved in the multicenter clinical studies on the prevention and therapy of type 2 and gestational diabetes, coordinated by the German Center for Diabetes Research (Deutsches Zentrum für Diabetesforschung).
Furthermore, we aim to reveal the pathophysiological role and predictive value of important hormones/biomolecules for the manifestation and progress of common metabolic diseases (i.e. type 2 diabetes, obesity, non-alcoholic fatty liver disease) in humans and mice and use metagenome-based approaches to develop novel strategies for the prevention and treatment of diabetes. In immunometabolism studies, we furthermore investigate the cellular and molecular mechanisms underlying the crosstalk of inflammation and metabolism in order to identify the role of inflammatory processes in obesity-associated metabolic diseases such as insulin resistance or type 2 diabetes. Another aspect of our research is the early detection of type 1 diabetes in newborns and the prevention of type 1 diabetes with oral insulin. The objectives of these studies are the immunoprevention of type 1 diabetes, which is primarily focus on preventing the autoimmune mediated destruction of beta cells and developing cellular markers that can be used to identify people at high risk for the development of type 1 diabetes at an early stage.